
Expediting the process of getting the claims paid shortens the account receivable days, and accounts receivable in healthcare increases cash flow. According to colburnhill.com dynamics is particularly obvious in the area of low balance claims, which have been generally viewed as worth only a cursory squeeze, and not given the full refolding treatment. Some organizations have consciously de-emphasized claims with payer balances as large as $5,000.
How to Optimize Accounts Receivable Management?

Proactive measures, robust training programs, and the use https://solidapparatus.mylearndash.com/a-guide-to-travel-expense-reimbursement-process/ of technology can empower providers to overcome AR challenges and focus on delivering quality patient care. With a strategic approach to AR management, healthcare organizations can ensure financial stability and long-term success. The days in A/R metric is the average number of days it takes for a provider to be paid for a service provided. This calculation gives hospital leaders insight into how well their revenue cycle is performing. A well-performing revenue cycle means better cash flow, lower collection costs, and less pressure on already overworked staff. By combining our medical billing expertise with advanced RCM solutions, we empower healthcare organizations to focus on patient care while we ensure seamless revenue flow.
Hospital Accounting: A Complete Guide for 2024
Over the last decade, we have been setting the benchmark, extending robust support to leading hospitals all around the country with excellent references. We have trained resources who have experience to use analytics and understand trends in what is rising your number of denials? One of the biggest advantage is that we are versatile with our presence across a wide spectrum of providers cutting across more than 28 specialties. It’s very complex and, because it relies on assumptions and estimation, it’s susceptible to errors and fraud. We also use different external services like Google Webfonts, Google Maps, and external Video providers.
- Hospitals often struggle with outdated AR workflows that lack prioritization.
- Furthermore, increasing the predictability of cash flow requires effective AR management.
- That leads to longer resolution times and more revenue slipping through the cracks.
- If healthcare staff that is responsible for billing are not trained properly then, they can make coding and billing mistakes which cause unnecessary spending.
- Since AR involves complex billing processes, it has a big impact on how well your practice runs and how financially stable it is.
- Moreover, you should consistently communicate with your patients about their overdue payments to enable timely reimbursements.
hospital financial benchmarks 2023
This elevated responsibility leads to a higher number of bad debts, which are bills that patients never end up paying. This is also the main reason for aged accounts receivable in the healthcare space, as an insurance company’s inability or unwillingness to accept a claim often leads to outstanding payments. Another challenge, adding to the complexity of A/R recovery is the rise in patient responsibility, which requires practices to chase patients directly to collect payments, not just the insurance firms.

Outsourcing vs. In-House Follow-Up: What Works Best for Unpaid Medical Claims?
- You should also have sufficient revenue to allocate proper resources for your processes.
- The process becomes even more challenging if a patient has moved or passed away.
- Taking proactive steps, such as improving follow-ups, claim scrubbing, and patient communication, can help bring down AR Days.
- Jacqueline LaPointe of revcycleintelligence.com says understanding complex payer contracts is key to ensuring timely, correct reimbursement and keeping a practice’s doors open.
- Health insurance plans are far too varied, they are regulated with contracts that payers sign with individual practices and health systems, and which periodically are renegotiated.
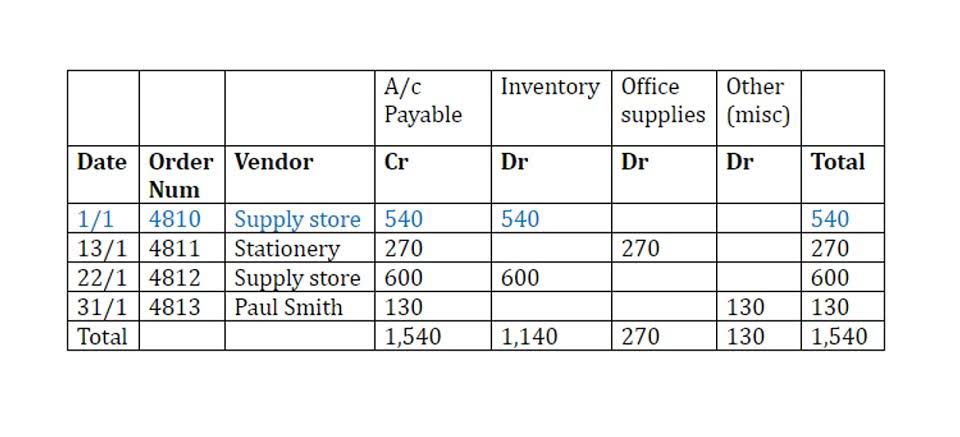
- Also dividing the total A/R by the average daily charges gives the days in A/R.
An ancillary effect is that patients and the public often don’t know what to expect in terms of care costs and may be surprised by practices such as balance billing. Healthcare providers need to track A/R medical billing frequently and analyze data every month. Checking consistently will help in pointing out issues and understanding setbacks. Organizations often view patient access departments as transactional, high-cost centers that connect patients with providers while generating bad debt and claims denials. Physicians often grow frustrated by the administrative burden and delays in care that poor patient access creates.
What Is Hospital Accounts Receivable Services?
When we ask questions about medical accounts receivable, we usually get answers like, “Oh, our AR is very low! Innovation and appropriate strategies are of paramount importance when it comes to efficient practice management. By constantly seeking out new ways to streamline processes and improve productivity, a practice can stay ahead of the competition and better serve its clients. Every member of your AR management team should understand the claim submission requirements of payors, coding regulations and guidelines, compliance requirements of HIPAA and other relevant legalities.

- Claim denials are one of the top culprits behind sluggish hospital accounts receivable performance.
- It is easier for you to first sort them out and then initiate their collection procedure.
- Claims that are lingering in your aging bucket for months are likely to be adjusted or denied, and may be worth very little in terms of reimbursement.
- Hospital accounts receivable services in healthcare refers to the amount of money a provider owes from patient and insurance.
- Measurement of Account Receivable is called “Days in AR” which represents the average time it takes to collect a bill.
Aging claims, denial delays, inefficient processes, and staffing issues all create hidden costs that directly impact your bottom line. Horizon Healthcare’s AR solutions are built specifically for providers facing these kinds of challenges. Hospital billing is an intricate process that requires in-depth knowledge of medical codes.
Unapplied Payments
In this blog about Healthcare Accounts Receivable Management, let’s see why it is important, how to measure it, and steps to improve it. In situations where the billing office of the health organization is not adequately staffed, it makes better sense to look for third party vendor support, so that the cash-flow is continual and ceaseless. Second, to reaffirm the importance of a strong relationship between patients and their healthcare professionals. Patients should be able to expect that their physicians will provide guidance about what they consider the optimal course of action for the patient based on the physician’s objective professional judgment. Another important aspect of AR management is having the most efficient software.
Physician Billing
To ensure seamless accounts receivable management, you need to foster a systematic culture of payment collection. You should use the right tools and approach to collect payments so that your patients don’t feel disappointed. Hospitals face several challenges with AR entry, including inaccurate data entry, managing high volumes of claims, and tracking denied claims. These issues can lead to delayed payments and backlogs, impacting cash How to Invoice as a Freelancer flow.

Be the first to comment